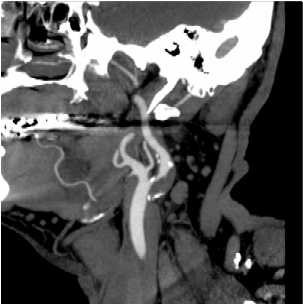
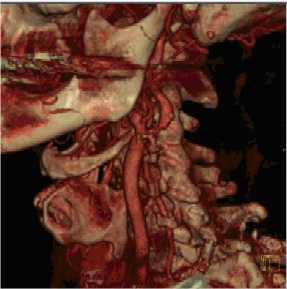
Narrowing of the carotid artery in the neck is a common cause of stroke in Western countries. The North American Symptomatic Carotid Endarterectomy Trial (NASCET) found endarterectomy to be beneficial in a highly select group of patients with symptomatic stenoses of greater than 70% severity with a reduction in the subsequent 2 year stroke rate from 26% to 9%.
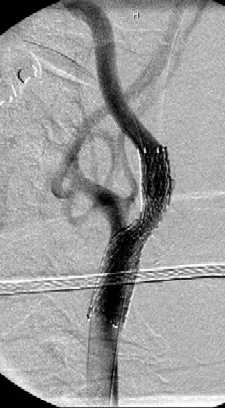
Carotid artery stenting (CAS) has evolved in the past decade as an alternative to CEA in high-risk patients. CAS is already viewed by some physicians as a true alternative to CEA without the potential surgical complications of tissue scarring, cranial nerve injury, and neck haematoma. The recently released CREST study would indicate that with skilled operators CAS is equivalent to CEA. Other studies have shown advantage to CEA when the operators had limited CAS experience.
The procedure is usually performed with the patient awake and lightly sedated. The patients all need medical preparation with anti platelet drugs, usually aspirin and Plavix. It is our practice to use a distal protection device whenever possible. These are placed beyond the narrowed segment and are designed to catch any material that may be dislodged into the circulation during the stenting procedure. If the narrowing is severe, an angioplasty may need to be performed before stenting. This "pre-dilatation" manoeuvre involves placing a small balloon across the narrowed segment and dilating the stenosis to facilitate placement of the stent. The stent can then be deployed and any residual stenosis may be angioplastied ("post-dilated") as required. The catheters and distal protection device are then carefully removed and haemostasis at the groin puncture site is usually achieved using an arterial closure device such as an Angioseal™ or Perclose®. Complications of the procedure are in the range of 2-7% depending on whether the stenosis is symptomatic, the patient age and co-morbidities as well as the morphology of the stenosis and arteries.
After the procedure the patient is usually kept in a high dependency or intensive care ward overnight. Blood pressure may need to be controlled. Antiplatelet therapy continues after the procedure with aspirin to continue indefinitely and Plavix for 3 to 6mths. A follow-up CTA is usually performed at 3-6 months to check for renarrowing inside the stent. This occurs in approximately 5% of patients.